Proton pump inhibitor (PPI) medications are one of most frequently utilised classes of medicines. Primarily used to treat gastro-oesophageal reflux disease (GORD), gastritis and peptic ulcer disease, use of these medications has risen sharply over the past two decades. In fact, utilisation has increased by over 1300% over this time! Commonly used PPIs include omeprazole […]
Category Archives: dysbiosis
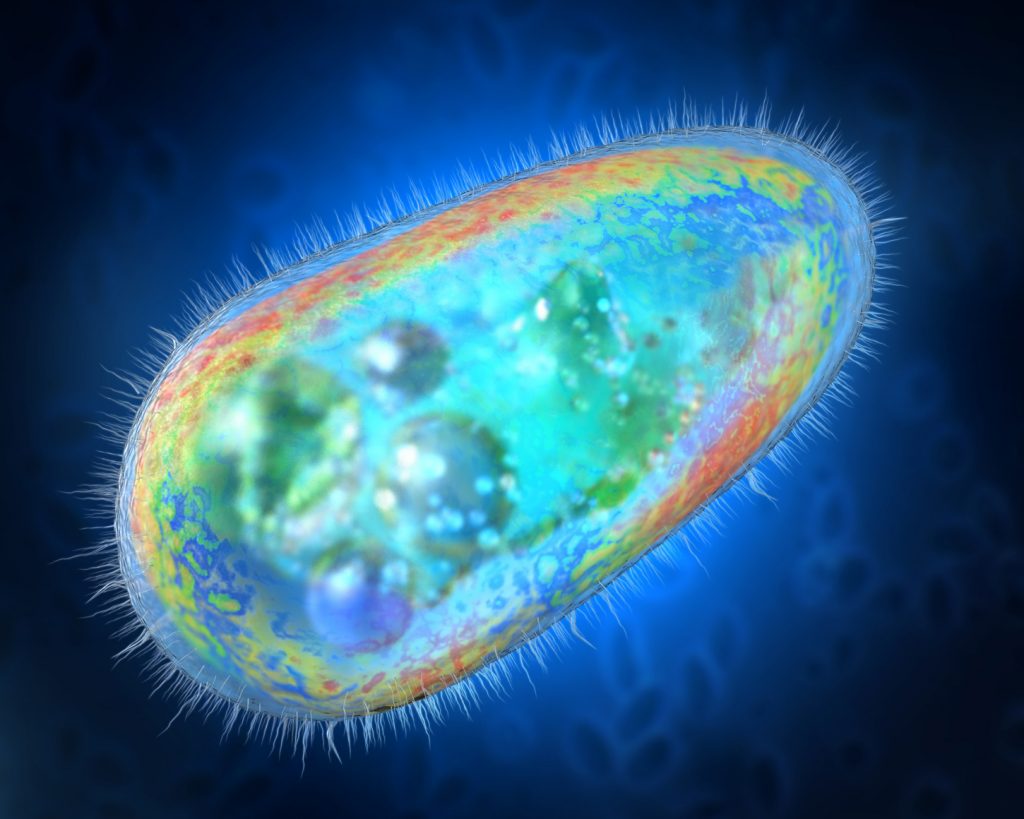
When preparing for my recent lecture at the 11th Herbal & Naturopathic International Conference – Using Herbal Medicines to Modify the Microbiota – I came across an interesting study that looked at the impact of dang shen (Codonopsis pilosula) on the gut microbiota – and specifically gastrointestinal concentrations of Desulfovibrio spp. – a key […]